PATHOLOGY LAB TRANSFORMS, RUNS 1M COVID-19 TESTS
Histopathology lab adapts its molecular capabilities to handle ever-greater numbers of SARS-CoV-2 tests
By Robert Michel | From The Dark Report Volume XXVIII No. 3 – March 1, 2021
CEO SUMMARY: Last spring, a histopathology lab in Illinois began running molecular COVID-19 tests and decided the clinical side of the lab would focus exclusively on PCR testing for COVID-19. The challenge was how to access a reliable source of test kits, reagents, and supplies to operate 24 hours a day, seven days a week. The answer came in the form of a multi-million-dollar lab supply contract that allowed the lab to perform more than one million SARS-CoV-2 tests within eight months.
IN THE 1950s TELEVISION SERIES OF THE SAME NAME, a narrator told viewers there were “eight million stories in The Naked City.” Today there may be eight million stories about COVID-19 testing, but few are likely to be as improbable as the one Reditus Laboratories has to tell.
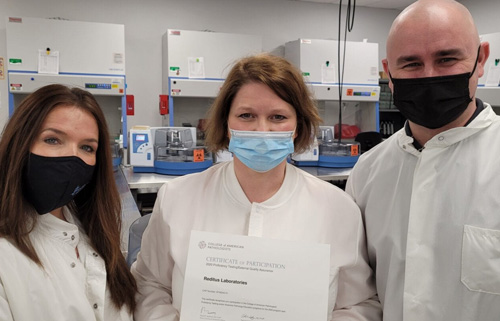
Founded in 2019, this moderate-sized histopathology lab in Pekin, Ill., started running polymerase chain reaction (PCR) tests for COVID-19 in April. Since then the clinical laboratory has focused exclusively on PCR testing while continuing to support its anatomic pathology business. Since the fall, Reditus has run 15,000 to 17,000 COVID-19 tests each day.
Million Test Milestone
“By late November, we hit our first million COVID-19 PCR tests,” Reditus CEO Aaron Rossi, MD, said in December. “Now, we’ve already performed 1.35 million tests, meaning we could hit our second million in the next few weeks.
“Just before the middle of April, we went live on one machine with our first PCR test for COVID-19,” Rossi added. “In those early days, we used the Thermo Fisher EUA test for the coronavirus. Within a few months, we had run several thousand tests, and now we’re tracking at a much higher level.”
For Rossi and the lab’s 250 employees, the journey from being a histopathology lab to running clinical lab tests for SARS-CoV-2 has been chaotic at times because testing volume has grown so quickly as a result of two strategies that Rossi employed.
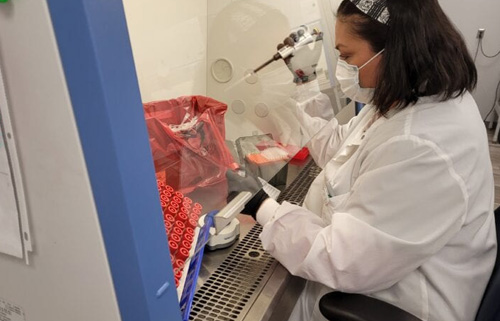
First, the clinical side of the lab has focused exclusively on PCR testing. Second, once it was running PCR tests, the lab needed to feed the beast, so to speak, every day. To accomplish that, Reditus, like every clinical lab, needed enough lab testing supplies to run those tests around the clock.
Rossi solved that problem by signing a multi-million lab-supply contract with Thermo Fisher. Under that contract, the lab has maintained a high-throughput strategy since April, while going from a few hundred tests per day to doing more than 600 tests per hour, or about 15,000 tests every 24-hours.
To accommodate the growing test volume, Reditus is increasing the size of its 14,000-square-foot Pekin lab to accommodate more PCR testing equipment, including six of Thermo Fisher’s QuantStudio 5 Real-time PCR Systems and eight of the KingFischer Flex Systems for molecular particle extraction.
By focusing exclusively on PCR tests, Rossi explained that the lab has been successful in testing for Illinois cities, towns, and state agencies. Since the spring, these clients have steadily increased their demand for COVID-19 tests. While test volume has risen and turnaround times have lagged occasionally, Reditus has reported most SARS-CoV-2 results in about 13 hours, Rossi said.
“We provide testing for municipalities and for the state of Illinois within about a 150- to 200-mile radius,” he reported. “For those clients, we’re very cognizant of our quality and turnaround time. To do that, we focus on quality over quantity. We don’t over-commit and under-deliver.”
Turnaround Times
Despite that goal, Reditus was in the news in May and again in August when some test turnaround times reportedly stretched to four and seven days and beyond, according to published reports.
For the state of Illinois’ Emergency Management Agency, Reditus has run drive-up testing sites in Bloomington, Peoria, and five other Illinois cities. Also, Reditus had a contract last year with eTrueNorth, a lab testing company operating drive-through testing sites nationwide under a contract with the federal Department of Health and Human Services. (See “Texas Company Operates 400 COVID-Collection Sites,” TDR, Aug. 24, 2020.)
“We struggled to meet the demand for COVID-19 testing when Illinois officials shifted from having the National Guard do some of the specimen collections to having us do that collection and testing,” Rossi said.
To ensure that the lab can add volume without slowing turnaround times, Rossi has not introduced any other form of COVID-19 testing that might divert attention away from PCR testing. The lab does not pool specimens, for example, and it has not introduced antigen, antibody, or saliva tests for SARS-CoV-2, he said.
‘Stayed in Our Wheelhouse’
“We never got involved in any other form of COVID-19 testing because we’re not in the screening business,” Rossi commented. “Instead, we stayed in our wheelhouse, which is diagnostic testing using PCR.”
Adding any other form of testing could jeopardize an operation that needed to stay focused on getting specimens in, testing those patient samples quickly, and getting the results out to patients and treating physicians, he explained.
“We’re sticking to a basic business plan that requires we take our time with each step in the process and make sure we do everything right,” noted Rossi. “When a lab runs 24/7 and receives 16,000 to 17,000 specimens a day, any type of workflow disruption can cause a massive back-up.
“If our lab’s workflow is disrupted for even a few hours, the backup can quickly rise to 8,000 specimens,” he warned. “When that happens, new specimens don’t stop coming in. Instead, we have a back-up lab if needed. No lab wants to be in the news for not getting results out in time.
News Coverage of Pandemic
“Everybody looks at COVID-19 as a celebrity, and the news people like to talk about all the bad stuff,” he added. Some of the nation’s largest labs have been in the national news when turnaround times for COVID testing ran over a week or more.”
Another reason Reditus could manage a steady increase in testing and large volumes of specimens for molecular assays is because the histopathology lab already had an operational and financial management system that could be adapted to support the clinical lab, Rossi explained.
Before the pandemic, Reditus was a fast-growing histopathology business that ran the LigoLab LIS (laboratory information system) and revenue cycle management systems. “That platform includes the modules we needed, not only for anatomic pathology but also for clinical laboratory and molecular diagnostics,” Rossi said.
Seamless Transition
“Having those capabilities in our LIS helped to make the transition from histopathology to COVID-19 testing relatively seamless,” he concluded. “When we started doing PCR testing, we already had significant operational and financial infrastructure in place to do that molecular diagnostics testing.”
In response to the outbreak of COVID-19 last winter, the team at Reditus Laboratories recognized an opportunity to achieve two important goals. The first goal was to support the community and the region with essential molecular SARS-CoV-2 testing done locally. The second goal was find new clients and accounts so that the lab could generate the cash needed to support SARS-CoV-2 testing while also keeping the lab financially stable throughout the course of the pandemic.
Illinois Pathology Laboratory Steadily Increased COVID-19 Test Volume by Adding New Clients
FOR REDITUS LABORATORIES CEO AARON ROSSI, MD, one key to introducing COVID-19 testing successfully was to add clients slowly and steadily.
“When we started SARS-CoV-2 testing last spring, we had three or four substantial accounts,” he said. “By doing testing for these accounts, we showed we were capable of doing COVID-19 testing even though we had never done that testing before.
“Within a few months, the State of Illinois needed more clinical laboratories to meet the demand for SARS-CoV-2 testing at community-based testing sites (CBTS),” noted Rossi. “Initially, we had one CBTS that sent us about 500 specimens a day under a state contract. From there, we slowly added more volume as additional state CBTS referred specimens to us.”
Today, about 75% of the lab’s COVID-19 test volume comes from 10 drive-through and mobile-testing sites for the Illinois Department of Public Health. The remainder comes from work for the state Department of Corrections, area hospitals, and long-term care facilities.
In the spring, Rossi and the Reditus lab team were establishing the processes needed to ensure that every part of the operation—from accessioning to reporting results—ran smoothly and efficiently. “Just like any lab trying to get off the ground, we had growing pains as we added more testing sites,” he commented.
As COVID-19 test volume grew, Rossi found that—as every other lab discovered—the need for a reliable source of reagents, testing supplies, and equipment was critical. “From the beginning, we had worked closely with Thermo Fisher,” he reported. “It seemed like they prioritized our lab, and so we asked for the supplies and equipment we needed, and they responded.
“From there, we started to build our rapport with Thermo Fisher and signed a contract so that we could be allocated the reagents we needed,” he noted. “After that, we discussed going to an exclusive reagent deal with them and that became a big leap for us. That was a $14 million contract in which Thermo-Fisher agreed to supply what we needed in reagents and other supplies.
“As a result of that supply contract, we never had any serious slow down or drop off in SARS-CoV-2 testing,” he said. “We never had a shortfall of reagents, pipette tips, plastics, or other consumables of any kind.”
Contact Aaron Rossi at a.rossi@redituslabs.com.
Link to the article – Histopathology lab adapts to handle PCR testing for COVID-19 (darkintelligencegroup.com)